PRP THEARPY VS DIABETIC FOOT
WHAT IS ROLE OF DIABETIC FOOT IN PRP?

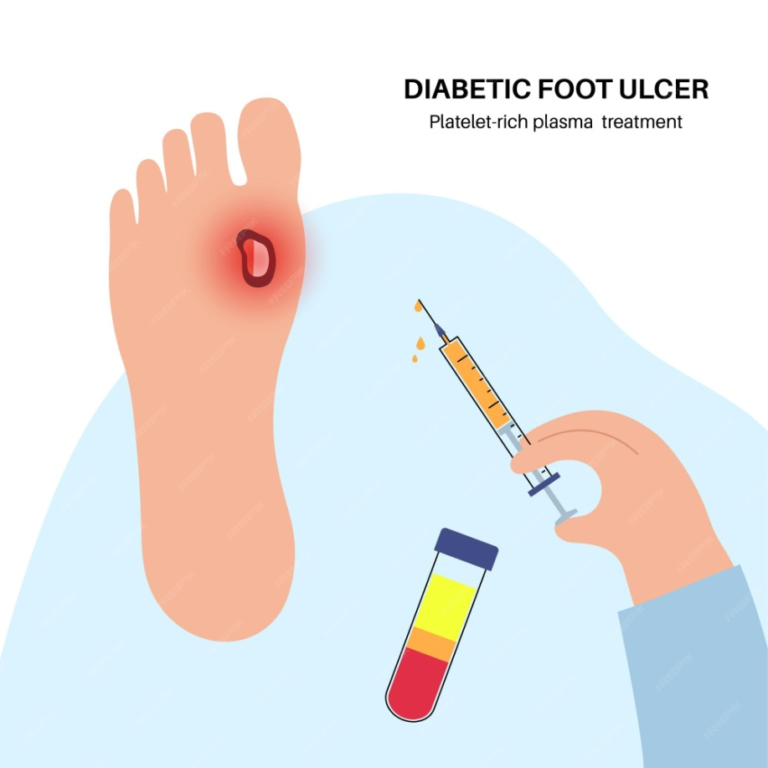
Diabetic foot with PRP refers to a treatment approach for diabetic foot ulcers that involves using platelet-rich plasma (PRP) therapy. Diabetic foot ulcers are open sores or wounds that commonly occur in people with diabetes due to factors like poor circulation and nerve damage.
WHAT IS THE PROCEDURE OF DIABETIC FOOT WITH PRP THEARPY?
1.Consultation and Assessment:
The process starts with a consultation with a experienced plastic surgeon.They’ll assess the diabetic foot ulcer, its severity, and the patient’s overall health to determine if PRP therapy is suitable.
2.Blood Collection:
If deemed appropriate, the next step involves drawing a small amount of the patient’s blood, typically from the arm, similar to a regular blood test.
3.PRP Preparation:
The collected blood is then processed in a centrifuge machine to separate the platelet-rich plasma (PRP) from other blood components. This concentration step increases the platelet count and growth factors in the plasma, which are crucial for wound healing.
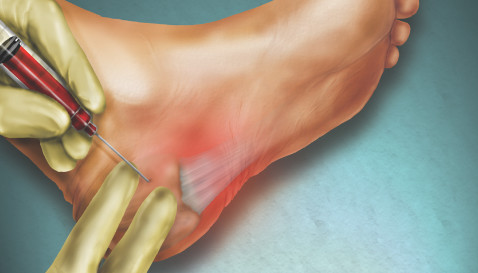
4.Application of PRP:
Once the PRP is prepared, it can be applied directly to the diabetic foot ulcer in various ways:
- Topical Application: The PRP may be directly applied to the wound surface.
- Injection: In some cases, especially for deeper or larger ulcers, the PRP might be injected into and around the ulcer site.
5.Bandaging and Follow-up:
After the PRP application, the wound might be dressed or bandaged appropriately to protect it. Patients are often advised on wound care techniques to follow at home and scheduled for follow-up appointments to monitor healing progress.
6.Additional Treatments:
PRP therapy is often part of a comprehensive treatment plan that may include other interventions like antibiotics,
offloading pressure from the affected area, managing blood sugar levels, and ensuring proper wound care to optimize healing.
7.Monitoring and Repeat Treatments:
Healing progress is closely monitored, and additional PRP treatments may be recommended based on the response to the initial therapy.
How effective is PRP therapy for diabetic foot ulcers?
PRP therapy has shown promise in the treatment of diabetic foot ulcers, but its effectiveness can vary among individuals and depends on several factors, including the severity of the ulcer, the patient’s overall health, and adherence to proper wound care.
1.Stimulating Healing:
The growth factors present in PRP can help stimulate tissue repair and regeneration, potentially accelerating the healing process.
2.Reducing Inflammation:
PRP may have anti-inflammatory properties, which can aid in controlling inflammation around the ulcer and promoting healing.
3.Enhancing Blood Vessel Formation:
PRP may support angiogenesis, the formation of new blood vessels, which is crucial for adequate blood supply to the wound for healing.
Are there any studies showing the benefits of PRP in treating diabetic foot wounds?"
Yes, there are several studies and clinical trials that have investigated the benefits of PRP (platelet-rich plasma) therapy in treating diabetic foot wounds. While the field of research is ongoing and results can vary, many studies have reported positive outcomes and benefits associated with using PRP for diabetic foot ulcers.
1.Improved Healing Rates:
Several studies have shown that PRP therapy can lead to faster healing rates in diabetic foot ulcers compared to standard treatments alone. This includes reduced wound size, improved tissue regeneration, and faster closure of the ulcers.
2.Reduced Infection Rates:
PRP therapy has been associated with lower rates of wound infection in diabetic foot ulcers. The antimicrobial properties of PRP might contribute to reducing the risk of infections and related complications.
3.Enhanced Tissue Regeneration:
PRP contains growth factors that stimulate cellular proliferation and tissue regeneration, potentially leading to improved wound healing outcomes.
4.Pain Reduction:
Some studies have suggested that PRP therapy might contribute to reducing pain associated with diabetic foot ulcers, enhancing the overall quality of life for patients.
5.Combination Therapy:
In many cases, PRP therapy is used in combination with other treatments (such as wound dressings, offloading devices, and infection management), showing synergistic effects and improved overall outcomes in wound healing.
What are the risks or side effects of PRP treatment for diabetic foot?
PRP (platelet-rich plasma) therapy is considered safe because it utilizes the patient’s own blood components, reducing the risk of allergic reactions or infections. However, as with any medical procedure, there are potential risks and side effects associated with PRP treatment for diabetic foot ulcers. Some of these include:
1.Pain or Discomfort:
Mild pain or discomfort at the injection site is common after PRP therapy. This usually resolves on its own within a few days.
2.Risk of Infection:
While the risk is low due to the use of the patient’s own blood, there’s still a slight risk of infection at the injection site. Proper sterile techniques during preparation and administration help minimize this risk.
3.Inflammation:
Some individuals might experience temporary swelling, redness, or inflammation at the site of PRP injection.
4.Bleeding or Bruising:
As with any injection, there might be a risk of bleeding or bruising at the injection site.
5.Allergic Reactions:
Although rare since PRP is derived from the patient’s own blood, there’s a minimal risk of allergic reactions.
6.Failure to Improve:
Not all diabetic foot ulcers respond equally well to PRP therapy. In some cases, the ulcers may not show significant improvement despite treatment.
7.No Guarantees:
PRP therapy, like many medical treatments, doesn’t guarantee complete healing or resolution of the ulcer. Response to treatment can vary among individuals.

List out the advantages and benefits of prp thearpy with diabetic foot ulcers?
1.Accelerated Healing:
PRP contains growth factors that promote tissue repair and regeneration, leading to faster healing of diabetic foot ulcers.
2.Enhanced Wound Closure:
It aids in the formation of new blood vessels and cell proliferation, which can facilitate the closure of chronic wounds.
3.Reduced Infection Risk:
PRP’s antimicrobial properties may lower the risk of infections in diabetic foot ulcers, improving the overall wound environment.
4.Minimal Side Effects:
As PRP is derived from the patient’s own blood, the risk of adverse reactions or rejection is low, making it a safe treatment option.
5.Non-Invasive Procedure:
The process involves collecting a small amount of the patient’s blood, processing it, and applying the PRP directly to the wound, which is less invasive compared to some other treatments.
6.Potential Cost-Efficiency:
Studies suggest that PRP therapy might reduce healthcare costs by potentially decreasing the need for more invasive procedures or extended hospital stays due to non-healing wounds.
7.Complementary Treatment:
PRP therapy can be used in conjunction with other standard treatments for diabetic foot ulcers, potentially improving overall outcomes.
Can PRP help in healing chronic diabetic foot sores?
PRP (platelet-rich plasma) therapy has shown promise in aiding the healing process of chronic diabetic foot sores or ulcers. Chronic foot ulcers in individuals with diabetes can be particularly challenging to heal due to impaired circulation, nerve damage, and other complications associated with diabetes.
Studies and clinical trials have indicated that PRP therapy may be beneficial in the treatment of chronic diabetic foot ulcers by:
1.Stimulating Healing:
PRP contains growth factors that can stimulate tissue regeneration and repair. These growth factors play a role in promoting cell proliferation and wound closure, potentially aiding in the healing of chronic ulcers.
2.Enhancing Blood Supply:
PRP may support angiogenesis, the formation of new blood vessels. Improved blood flow to the affected area is crucial for supplying oxygen and nutrients necessary for healing.
3.Reducing Inflammation:
PRP has been suggested to have anti-inflammatory properties, which can help in controlling the inflammatory response around chronic ulcers, facilitating the healing process.
4.Accelerating Wound Closure:
Some studies have reported faster wound closure rates in chronic diabetic foot ulcers treated with PRP compared to standard treatments alone.
However, while there’s growing evidence supporting the potential benefits of PRP therapy in healing chronic diabetic foot sores, individual responses to treatment can vary. Not all chronic ulcers may respond equally well to PRP, and factors such as the ulcer’s size, depth, location, and the patient’s overall health can influence the outcomes.
How long does it take to see results with PRP treatment for diabetic foot ulcers?
The time it takes to see results from PRP (platelet-rich plasma) treatment for diabetic foot ulcers can vary significantly among individuals. Factors such as the ulcer’s severity, the individual’s overall health, adherence to treatment protocols, and other medical considerations can influence the healing timeline.
In general, some individuals may start to observe improvements within a few weeks to a couple of months after starting PRP therapy for diabetic foot ulcers. These improvements might include:
1.Reduction in Wound Size:
The ulcer may start to decrease in size, which is an initial sign of healing.
2.Improved Tissue Regeneration:
PRP therapy might stimulate tissue regeneration, leading to healthier granulation tissue formation in the ulcer area.

3.Decreased Pain or Discomfort:
Some individuals might experience a reduction in pain associated with the ulcer as the healing process progresses.
However, it’s important to note that complete healing of diabetic foot ulcers often takes time and might require multiple PRP treatments in combination with other wound care interventions. For more chronic or severe ulcers, it could take several months to achieve significant healing or complete closure.
Consistency in following the recommended treatment plan, including proper wound care, managing underlying conditions like diabetes, offloading pressure from the affected area, and regular follow-up with healthcare professionals, plays a crucial role in the healing process.
Patients should maintain realistic expectations and understand that individual responses to PRP therapy can vary. Consulting with experienced plastic surgeon like DR.A.SARAVANAN specializing in wound care or diabetic foot management can provide a better understanding of the expected timeline for healing based on the specific circumstances of the individual’s condition.
WHY I CHOOSE ARUMEEN AESTHETIC CENTERE FOR PRP THRARPY WITH DIABETIC FOOT ULCER?
Choosing a specific center or clinic, like Arumeen Aesthetic Center, for PRP therapy for foot ulcers involves considering various factors to ensure the best possible treatment and care:
Our centere treated specialization in wound care, diabetic foot management, or regenerative medicine.
DR.A.SARAVANAN is experienced plastic surgeon and one of the specialist in diabetic foot ulcer treatment And we have a track record of successfully administering PRP therapy for diabetic foot ulcers.
Arumeen center’s reputation, patient reviews, and success rates with PRP therapy specifically for diabetic foot ulcers. A center with a history of positive outcomes and patient satisfaction might instill confidence in their ability to provide effective treatment.
Ensure that the center maintains high standards of cleanliness, safety protocols, and uses state-of-the-art equipment for PRP therapy.
The facility’s environment should be conducive to providing safe and effective treatments.
Who Look for centers that offer personalized treatment plans tailored to individual patient needs. A thorough evaluation of your condition and a customized approach to PRP therapy can enhance its effectiveness.
It’s crucial to feel confident in our center’s ability to provide effective treatment and support throughout the healing process.


